Last week, the Trump administration announced that it would allow individual states to place work requirements on Medicaid recipients. Central to this announcement was the promise that this measure would be aimed at “able-bodied” people, assuring potential critics that pregnant women, children, the elderly and disabled enrollees would not face the same requirement. Kentucky Gov. Matt Bevin (R) immediately enacted the work requirement, threatening to drop 400,000 Kentuckians from Medicaid if the courts blocked his policy.
For proponents, it only makes sense: requiring mentally and physically fit people to work in exchange for their health-care coverage, they argue, will help foster a sense of self-reliance and curtail the ill effects of living on the public dole. But defining able-bodiedness is far from straightforward, and, historically, determinations of health and ability have been made by nondisabled people in positions of power, often at the detriment of disabled people.
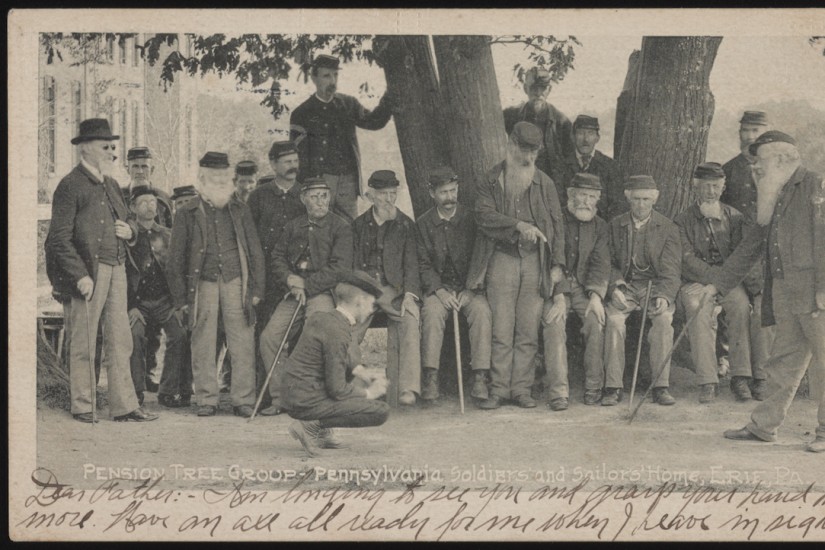
The idea that charity enables perfectly healthy, lazy people to live off the toil of hard-working citizens has been around far longer than federal entitlements. Indeed, the idea was already so deeply held that even the federal pension system, created to support sick and wounded Union veterans in the wake of the Civil War and arguably the first American welfare program, was designed to prevent creating a population of dependents.
Like the Trump administration’s change to Medicaid, avoiding a culture of dependency in the federal pension system hinged on able-bodiedness. Until 1890, pensions were available only to men with wartime disabilities, which were assessed by doctors and graded on a scale.
The scale was based on the amount of manual labor a disabled veteran could still perform. Old soldiers with ailments that made it more difficult or impossible to work received higher payouts, with smaller payouts granted for impairments considered less severe. Men sufficiently able-bodied to work received no pensions at all.
This distinction seemed — and still seems today — straightforward. But the problem was, and is, one of power. What exactly did “able-bodied” mean, and who had the power to make that decision?
For Civil War veterans, this often came down to the visibility of their disability. Highly visible disabilities were the easiest to categorize. A missing leg would obviously affect a man’s ability to perform manual labor profoundly; a missing toe perhaps less.
For nondisabled people, these readily apparent ailments were self-evident. They also carried a greater cultural cachet. Everyone understood what it meant to sacrifice an arm or leg to the glory of the Union. They were reminded regularly by sentimental literature and illustrations that portrayed amputees as heroes.
But how much did chronic diarrhea affect a man’s ability to work? How would pension clerks categorize something like intermittent fever, caused by contracting malaria while in the service, which got better and worse in cycles? Was such an ailment really worthy of the gratitude — and the cash — of the nation?
Not only were nonvisible disabilities difficult to define and categorize, they also raised the specter of malingering, or feigning impairment to bilk the U.S. government out of cash. How could the government be sure that a veteran claiming chronic headaches or gastrointestinal distress was telling the truth? The underlying fear was exactly that of current critics of Medicaid: that able-bodied men were passing themselves off as invalids for a handout.
The result was a conflict between the Pension Bureau and veterans, each claiming the right to define what it meant to be disabled and worthy of state support. To combat what they perceived as fraud in the system, doctors and clerks fell back on popular notions of disability and able-bodiedness to weed out fraudulent cases. These assumptions were heavily influenced by social and cultural assumptions about race and gender.
Veterans, they believed, should be ideal specimens of white American manhood. After all, these were the men who had just saved the Union. They expected even the most impaired men to carry their wounds with cheerful resolve, not betraying any suffering or fear. Even seeking out a pension seemed to prove to pension skeptics that a veteran was less worthy — after all, a true citizen-soldier fights without expectation of reward.
To give the Pension Bureau what it seemed to want, old soldiers with nonvisible disabilities learned to mask symptoms to create the appearance of able-bodiedness. But appearing able-bodied to display their masculinity was a double-edged sword in more ways than one. Working hard to appear strong and able often exacerbated the health problems plaguing these veterans.
Additionally, trying to meet this cultural standard created a Catch-22: When pension doctors examined them, they doubted the veracity of veterans’ claims of pain, sickness or physical difficulty — precisely because they appeared able. How could a man appear fit, while also being disabled? Even in their written applications, veterans had to try to convince bureaucrats that, despite appearances, they really were disabled. Clerks and doctors, however, didn’t accept veterans’ testimony. Soldiers with nonvisible or difficult to define ailments received very small pensions or were rejected altogether.
Black veterans faced an even more difficult situation, as those adjudicating their pension cases often held racist notions that black men were inherently physically and mentally inferior, not to mention inclined toward sloth and trickery. Black soldiers with even the most carefully documented nonvisible ailments, such as lung or heart disease, were rejected or received minimal payments.
Though over a century has passed since Civil War veterans fought for their right to federal support, the problems those disabled soldiers faced remain very present. Defining “able-bodied” is far from simple. Supporters of this new measure will argue that the matter can be easily settled by differentiating between Medicaid recipients on Social Security Disability and those who are not, but not all disabled people use SSD. How will states determine what it means be disabled or able-bodied — and, perhaps more importantly, who will have the power to make that determination?
Given the system in place, one that distrusts the accounts of people applying for disability, disabled people will be punished by the continued distrust of nonvisible disabilities. Those who point to their experience of their own bodies to insist that they are unable to work while appearing healthy will be accused of malingering and trying to game the system. Black Medicaid users will undoubtedly feel the most severe effects, as studies demonstrate that doctors continue to believe that black people have a higher pain tolerance and are more likely to commit entitlement fraud or feign disability.
And it’s not just the inherent visibility or invisibility of a disability that’s at play. There remains intense social pressure to appear nondisabled. The stigma attached to mental illness means that people often do their best to hide the symptoms or are discouraged from discussing it openly.
People with chronic illnesses are encouraged to “power through” or “buck up” when fatigue and pain make it difficult to get through the day. Disabled people will find themselves in a double-bind: If they successfully meet societal pressure, state bureaucrats will subsequently assume them able enough to work for their benefits.
Just like the Union veterans who struggled to prove they were disabled enough, Medicaid recipients will be forced to prove that they are too disabled to be required to work. And like those veterans, many will struggle to explain invisible symptoms and ailments to nondisabled people in positions of power. Sadly, the result will be more disabled people losing their much-needed health-care coverage.